Ever experience having a parched mouth? And to alleviate the dryness, do you require any kind of oral oasis? If you feel this way, you may have xerostomia, often known as dry mouth. Dry mouth, a frequent oral health disorder linked to less saliva, can cause problems with how your mouth works and major oral health problems.
The effects of a mouth moisturizer can mimic a momentary oasis for dry mouth. We’ll give you the lowdown on mouth moisturizers so you can make the best decisions for your circumstances.
What results in oral dehydration?
More than one individual has the sensation of having a dry mouth. Simply put, the mouth is dehydrated. This triggers a slight increase in saliva production, accompanied by discomfort in the oral cavity. Therefore, it’s crucial to rehydrate promptly. You’ll restore a positive attitude and proper oral equilibrium in this approach.
A dry mouth is an indication of dehydration. This is brought on by a number of unique causes. Water dehydration is the major cause of xerostomia. In other words, consuming this beverage in even a small amount prevents the tongue from retaining moisture. Additionally, the mouth cavity becomes dry after taking some drugs. These include analgesics or hypnotics, which have the side effect of drying out the mouth.
This soreness may also be brought on by a chronic illness, a periodontal condition, or an immunological disorder. Finally, xerostomia is caused by an issue with the salivary gland. The majority of the time, this final one emerges at night. You’ll likely have a strong urge to drink a lot of water, as well as a tendency for your mouth to feel quite pasty. This will be followed by a challenge with readily chewing food and the emergence of some fissures.
These will be evident at the level of the lips and hurt. Dehydration in the mouth can be detected by bad breath. You can see the dentist to find the cause of the issue as soon as these symptoms start to occur.
Guidelines for maintaining oral moisture
In order to properly keep your mouth moisturized, there are a number of techniques.
Maintaining oral hydration
Your mouth can be hydrated in the first step by being humidified. Indeed, water will give the mucous membranes of this cavity the essential hydration. This fluid is capable of performing the same function as saliva. The key argument in favor of drinking water frequently is this. Make sure the temperature is not excessively high or low.
You can, however, choose between employing a water or synthetic saliva sprayer. The nerves that power the salivary glands are stimulated by this accessory. If you have a history of respiratory issues, a physician must recommend the use of oral moisturizer due to the hazards involved.
Saliva activation with certain workouts
It is possible to produce saliva by following some fairly basic procedures. You may do this by chewing sweets or gum. If at all feasible, make them without sugar and mint-flavored. With the aid of a fresh breath, the salivation process may then proceed in the best manner possible. Additionally, several fruits and vegetables have the capacity to encourage salivation on a regular basis.
Reducing the use of tobacco
Smoking damages heart and lungs. Using of tobacco not only affects will eventually impact your oral health. The chemicals employed in its synthesis, change how saliva is produced in the mouth. Tooth decay and other oral problems are consequences of this dry mouth.
Proper dental care
Oral hygiene is one of the key habits to having a moisturized mouth. This will prevent xerostomia-related disorders from developing. These include periodontitis, gingivitis, plaque, and tartar. For this, brushing your teeth after each meal is necessary. Use toothpaste that doesn’t have a lot of fluoride when doing it.
This item could harm your salivary glands and gums. As recommended by the dentist, you might use mouthwash or dental floss to optimize your brushing technique. It’s crucial to refrain from using an alcoholic rinse solution.
The Foundation and Benefits of Mouth Moisturizers
Mouth moisturizers work as a replacement for saliva to treat dryness. A mouth moisturizer provides advantages even if it isn’t a perfect substitute for the healthy saliva your body generates. An oral moisturizer can temporarily alleviate that dry mouth feeling by putting a protective coating of moisture on your oral tissues.
Several medical sites suggest using a xylitol-containing over-the-counter mouth moisturizer. For this crucial component in any mouth moisturizer you purchase, check the label. You may also inquire about recommended or prescribed moisturizing products for dry mouth with your dentist.
Simply moisturizing your mouth for a few seconds helps alleviate the symptoms of dry mouth. Because switching from “Ugh” to “Ah!” Some advantages of dry mouth moisturizer include:
- They’re portable, so you can moisturize your mouth while you’re on the go.
- You can use mouth moisturizers as often as needed, depending on the specific product – some are available via prescription. (For some products, your dentist or doctor might provide instructions on how often to use a mouth moisturizer daily.)
- Hydrating your mouth can alleviate symptoms of dry mouth, like speaking challenges, eating discomfort, or swallowing difficulties.
- You can lessen your risk of developing infections, gum disease, and cavities. Mouth moisturizers aid in preventing the bacterial overgrowth that causes these oral health issues.
Long-Term Remedies for Dry Mouth
Moisturizers for dry mouth are a nice short-term solution, but they are not a dry mouth cure. The oral moisturizer’s benefits will eventually wear off, and sadly, your mouth will feel dry once more.
Visit your dentist and doctor so they can determine the underlying reason for your dry mouth and treat it for long-term comfort. Among the several underlying factors that contribute to dry mouth are:
- Anxiety and stress
- Dehydration
- Medication side effects
- Neurological and autoimmune problems
- Illnesses including diabetes, addictions, and sleep difficulties
Oral Care and Dry Mouth
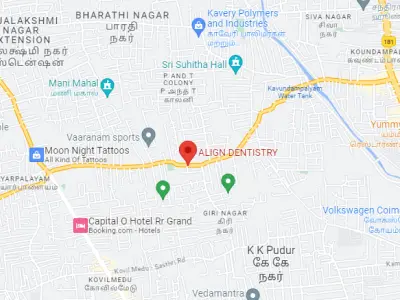
In the event of experiencing dry mouth, it is highly recommended to counteract it by employing an oral moisturizer. Nevertheless, it is crucial to complement this action with consistent dental care practices and regular biannual dental check-ups. Given that dry mouth elevates the likelihood of developing cavities and other oral health complications, upholding a stringent oral hygiene regimen is of utmost importance.
A dry mouth moisturizer is an easy approach to temporarily control the symptoms of dry mouth. But for long-term relief and to rule out any underlying problems, make sure you see a doctor.